What is Pharmacogenomics?
Pharmacogenomics is the study of how a person’s genetic makeup determines his or her response to medications. The effects of medications vary from person to person, and to some degree depend on variations within genes. This is one of the reasons why a medication may work well for some people and not for others, or why some people experience negative side effects while others do not.
The three major drug effects that pharmacogenomics attempts to predict are efficacy (how well a drug works), toxicity (negative side effects), and dosing (the correct amount of a drug to administer to a patient).
Pharmacogenomics
Personalized Therapeutics Unique to Each Patient
The cornerstone of pharmacogenomics rests on the identification of three pivotal drug effects: efficacy, toxicity, and dosing. Through meticulous research, we endeavor to predict these factors with unparalleled accuracy, revolutionizing the landscape of medical care. In contrast to the obsolete “one size fits all” approach that dominated the past, our approach embraces personalization, empowering clinicians to pick medications that resonate with each patient’s genetic profile.
Efficacy
How well the drug works given the patient’s medical condition and genotype?
Toxicity
What are the side effects of the drug and how can we minimize the adverse effect for the patient?
Dosing
How can we ensure the administration of the optimal dosage without the risk of overdosing?
The promise of the right treatments, at the right time, to the right person.
Until recently, medications were developed and administered in a “one size fits all” approach to meet the needs of an “average” patient. With the help of personalized research, clinicians have the ability to select the medications that work best for each patient.
Individualized drug therapy based on a person’s unique genetic makeup is desirable because of the variability of patient response to medications and the potential for life-threatening drug toxicities; adverse drug reactions are one of the leading causes of death in the United States. If clinicians could better predict which individuals are at risk of suffering drug-related toxicities, while also identifying those most likely to benefit, then the overall care of patients could be improved considerably.
Our Dedication to Personalized Therapeutics
At The Center of Personalized Therapeutics, we envision a future where treatments are not only effective but are also administered precisely when needed, to precisely the right individual. The power of pharmacogenomics opens the door to a new era of healthcare, where each patient’s genetic uniqueness becomes the cornerstone of their well-being.
We unravel the secrets of new genetic associations that profoundly influence how patients respond to medications. For instance, our ingenious team unearthed a variant within the KDR gene that holds the key to understanding patient responses to the cancer medication, pazopanib.

Our Approch
- By studying the genetic variations that impact drug metabolism, efficacy, and toxicity, pharmacogenomics equips clinicians with invaluable insights to tailor treatments precisely to a patient’s unique genetic makeup.
- Armed with this knowledge, healthcare professionals can confidently administer the ideal dosage, striking a delicate balance between therapeutic effectiveness and the avoidance of harmful side effects.

Deciphering Genetics and Drug Response
The very essence of precision healthcare lies in acknowledging the profound variations that exist between patients. As we delve deeper into the realm of pharmacogenomics, we are confronted with the exhilarating yet daunting task of deciphering the intricate language of genes, seeking hidden clues that dictate drug responses and therapeutic outcomes.
Genotyping
Pharmacogenomic studies are conducted based on patient genotype data.
Projects
The Center initiated multiple project to utilize pharmacogenomic discovery research in the clinic. The 1200 Patients Project is a great example of implementation research.
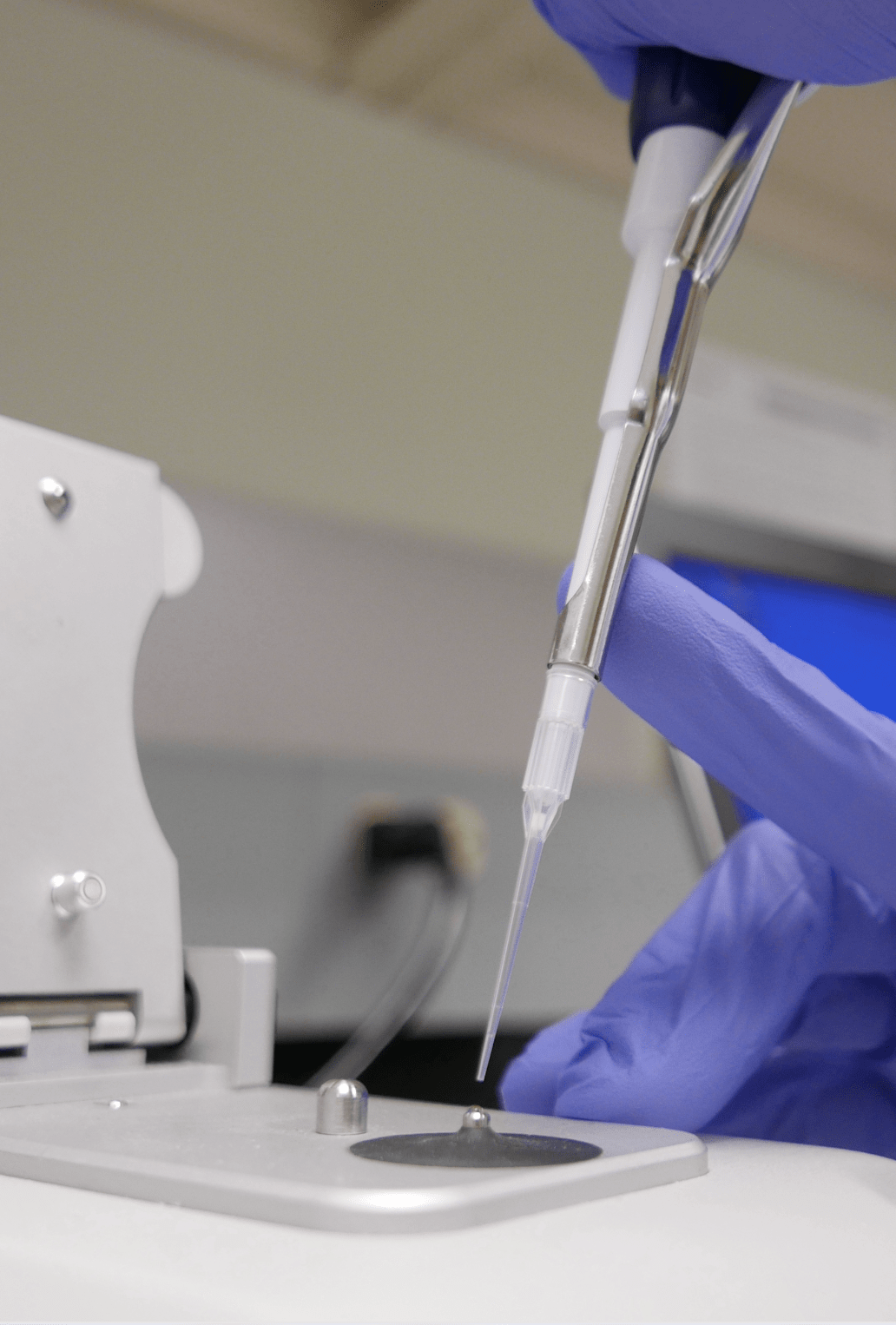
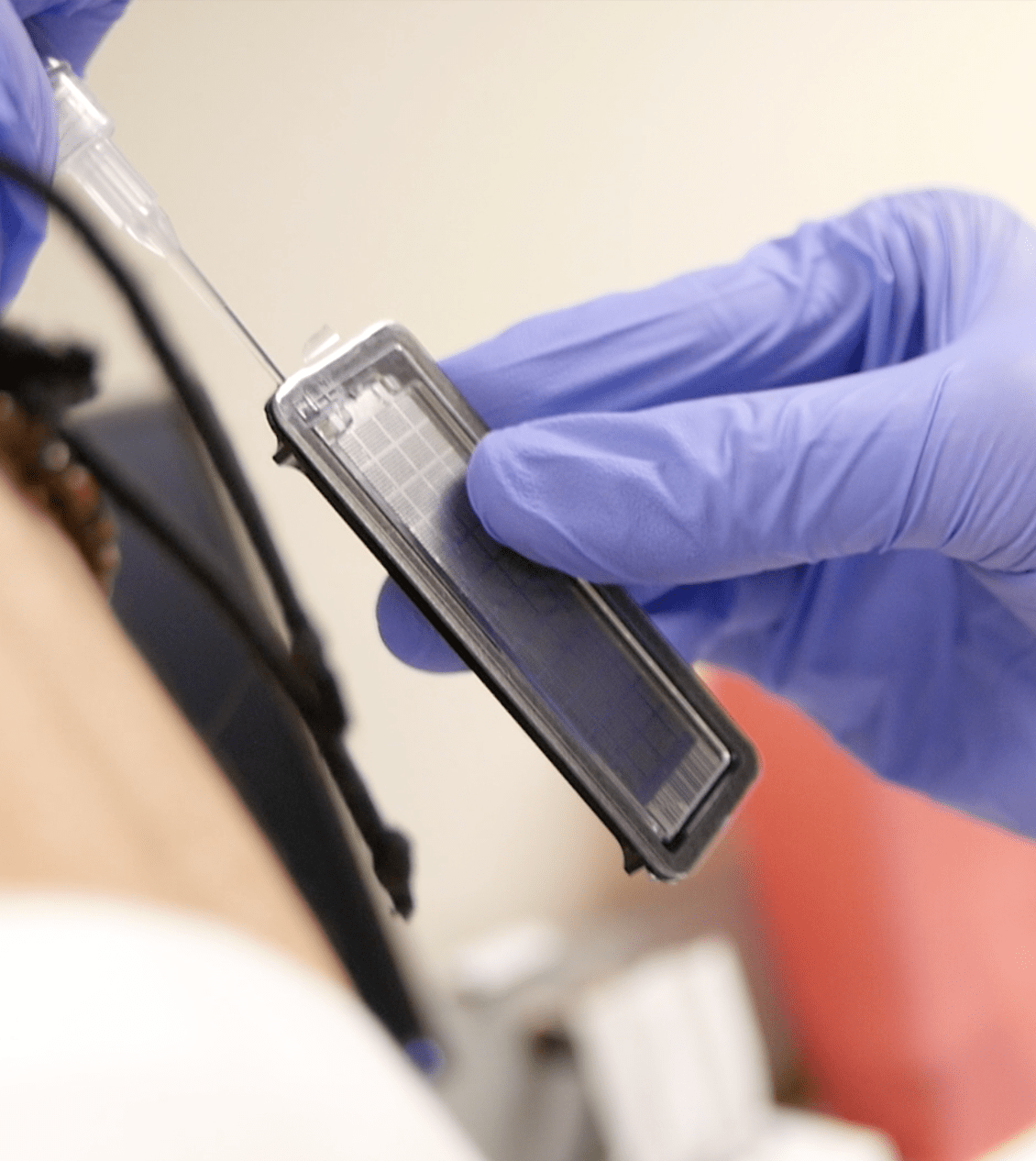
Laboratory
The Center for Personalized Therapeutics, in conjunction with the Pathology Department, has developed an in-house Clinical Laboratory Improvement Amendments (CLIA) certified laboratory for pharmacogenomics testing.
Privacy
The CPT understands that patient information is highly sensitive and takes care to ensure patient privacy and security.
Integrating Patient Genetics into Cutomized Healthcare.
At The Center for Personalized Therapeutics, we are embarking on an extraordinary journey to revolutionize patient care through the power of pharmacogenomics. Our groundbreaking research in pharmacogenomics spans two remarkable levels: Discovery and Implementation.
Pharmacogenomic Discovery
Pharmacogenomic discovery research seeks to find new genetic associations that affect patient responses to medications. For example, CPT members identified a variant within the KDR gene that affects patient response to pazopanib, a cancer medication.
Medical Implementation
Our implementation research attempts to find ways to utilize pharmacogenomic discovery research in the clinic. For example, in The 1200 Patients Project, we constructed an online Genomic Prescribing System (GPS) for clinicians so that they can easily use patients’ genetic information when making medication decisions.
Frequently Asked Questions
Contact Us
How does pharmacogenomics research translate to clinical practice and better healthcare?
The Center initiated multiple project to utilize pharmacogenomic discovery research in the clinic. The 1200 Patients Project is a great example of implementation research. In this project, we have synthesized previous pharmacogenomic research to build an online Genomic Prescribing System (GPS) to be used by clinicians so that they can easily use patients’ genetic information when making medication decisions.
Where does data for pharmacogenomic research come from?
Pharmacogenomic studies are conducted based on patient genotype data. Genotyping patients accurately is a primary challenge to pharmacogenomic research. To address this challenge, The Center for Personalized Therapeutics, in conjunction with the Pathology Department, has developed an in-house Clinical Laboratory Improvement Amendments (CLIA) certified laboratory to do pharmacogenomics testing. Running this genotyping platform in an in-house CLIA lab allows the CPT to genotype patients quickly and accurately, so clinicians can promptly access high-quality information.
How should clinicians get involved with pharmacogenomic studies?
Another barrier to pharmacogenomic implementation research is clinician and patient knowledge. Clinicians may not know when a pharmacogenomic test is available for a certain drug, for example. The CPT works to provide informative materials to clinicians and patients to educate them on the benefits and uses of pharmacogenomics.
How does the Center protect patient privacy?
The CPT understands that patient information is highly sensitive and takes care to ensure patient privacy and security. The 1200 Patients Project, for example, has earned the highest Certificate of Confidentiality from the National Institue of Health, which protects patient genetic information and guarantees that it cannot be distributed to any external institutions.
